National Rural News Source, The Daily Yonder, Writes Story On Ramifications Of CRNA Lawsuit
Alaska's Tribal Health Organizations Are Essential, And Powerful Story by Peter Heckendorn, Daily Yonder, July 31st, 2024 Robert Mars...
Alaska's Tribal Health Organizations Are Essential, And Powerful
THE DAILY YONDER'S STORY FOLLOWS:
Rural Alaska depends on healthcare services provided by tribal nations. This spring, the state's Supreme Court gave these organizations sovereign immunity, a decision that has ramifications for patients, providers, and rural communities.
In May of 2019, Yvonne Ito sued her former employer, Copper River Native Association, for wrongful termination after she was fired from her job overseeing a program helping senior citizens.
Copper River is a nonprofit tribal health provider and the primary healthcare organization for Native and non-Native communities alike in the Copper River Basin in East Central Alaska.
Laura Wolff, the Assistant Attorney General who filed a brief in support of Ito, believes the decision leaves the thousands of workers at those clinics in a tough spot. THOs that meet the new “Ito” test and are exempt from prosecution in Alaska must decide if they want to “waive sovereign immunity and be subject to suit by employees for violations of law. Otherwise, employees will have no legal remedy for such violations,” wrote Wolff in an email to the Daily Yonder.
The impact of the ruling will be felt throughout Alaska, where tribal health consortia are the primary source of healthcare for both Native and non-Native Alaskans in rural areas. Most states have some form of tribal healthcare, and tribal health sovereignty is an important issue throughout the country.
But no state has made tribal health the cornerstone of its statewide healthcare network the way Alaska has. In most villages and towns, tribal health consortia represent the only source of care. Amid national obstacles to effective, low-cost rural healthcare; some wonder if the ruling in Alaska could portend a larger shift in tribal healthcare across the country.
A Dearth of Dentists, Doctors, and Roads
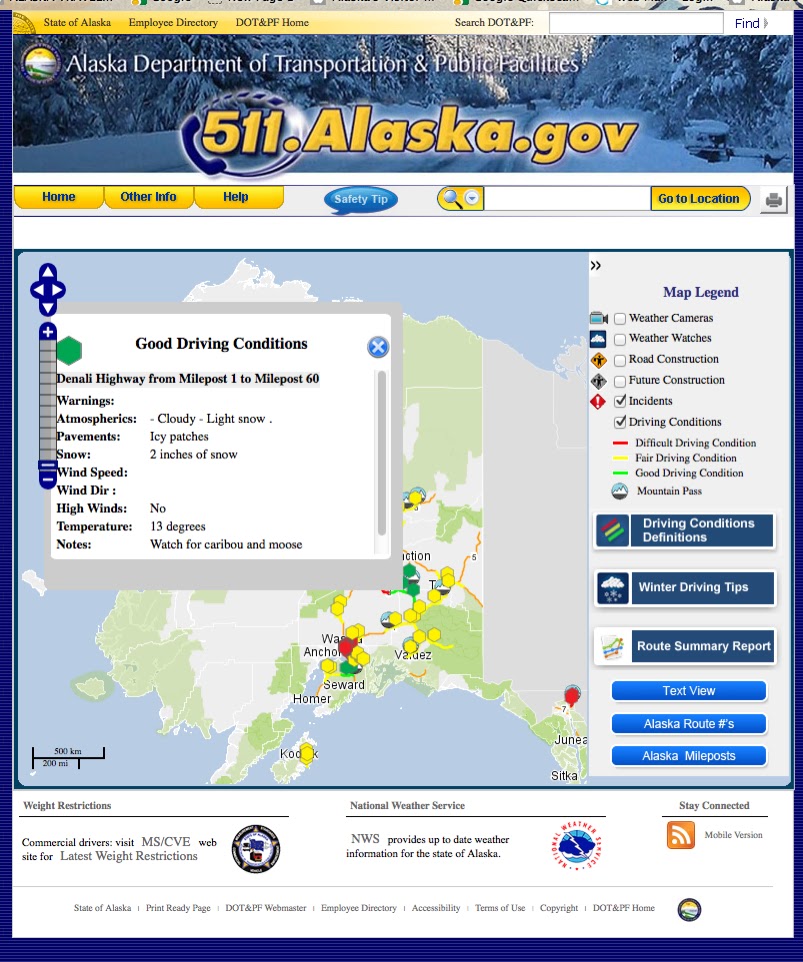
Tribal health consortia fill a unique need for healthcare in Alaska. Alaskans spend more on out-of-pocket healthcare costs than any other state. Over 80% of the state is not connected to a road system. It’s difficult to recruit providers to live and work in such remote locations, so clinics in Alaska often rely on mid-level practitioners from the communities themselves. Many lower-48 models of care don’t translate to the 49th state.
Zazell Cummings, who is Inupiaq and grew up near Kotzebue, Alaska, said that she decided to become a dental provider after a dentist broke a needle in her brother’s mouth while trying to fix his toothache in Anchorage. Cummings’ mother called off the procedure midway through and packed the family up to see a dentist they knew in Fairbanks, a six-hour drive away.
“The dentist was just not very nice. If my mom says someone is a jerk, that’s really bad,” she said.
The experience taught Cummings the importance of culturally, as well as medically, competent care. Cummings went to dentistry school so that she could provide both to her community. Today, she works for the Maniilaq Health Center, one of the state’s 17 major tribal health consortia.
Ahead of the Curve on Rural Solutions
Shea Seigert is the Senior Manager for External Relations at Alaska Native Tribal Health Center (ANTHC), the largest THO in the country and the center of Alaska’s “wheel and spokes” model of tribal health. From ANTHC spokes of the healthcare “wheel” radiate out into regional healthcare facilities, sub-regional clinics, and local community health aides. Seigert said that helping rural Alaskans navigate this system to get the care they need often necessitates innovation amidst a scarcity of resources.
“When you’re talking about communities that are some of the most remote in the world that experience some of the harshest weather conditions and some of the coldest temperatures, you have to get creative with your approach about how to build these systems,” said Seigert.
Two of the Alaska Native Tribal Health Center’s most impactful long-term investments are telehealth and community health aides. Long before the pandemic, Alaska was using virtual healthcare to connect urban doctors to remote patients. Tribal Health has also relied heavily on the Community Health Aides Program (CHAP), which equips rural Alaskans (who may not have more than a high school degree), to provide basic medical care to their community. Today, much of rural Alaska relies on the combination of telehealth and CHAP, in which health aides on the ground work together with supervising doctors and dentists in a central location to provide care.
In the first ten years of the dental health aide program, the proportion of rural Alaskan children with access to dental care doubled. Cummings confirmed the significance of these initiatives in increasing access to care. “I remember as a kid, dentists would come maybe once a year. Now each village sees a dentist more than once a year, and we have full-time providers here in Kotzebue,” she said.
'Arms of the Tribes'
The Copper River Supreme Court case brought up long-standing arguments about oversight of Alaska’s THOs.
Yvonne Ito sued Copper River for wrongful firing after she advocated against harassment and workplace wrongdoings, and Copper River immediately moved to dismiss the suit on the basis of sovereign immunity. “Tribes are sovereign dependent nations within the United States. This means in U.S. courts, tribes have many of the same rights as other nations and individual states, and cannot be sued without their consent,” said Richard Monkman, a lawyer who helped represent the Copper River in the Supreme Court case.
But it hasn’t always been this way. “20 years ago the Alaska Supreme Court took a different tack,” he said.
In a 2004 case, Alaska’s Supreme Court drew lines between tribal organizations and the tribes that ran them, excluding health consortia from sovereign immunity. In that case, the court relied on the “financial insulation” test: if the tribe’s assets would not be financially affected by a lawsuit against the organization in question, then that organization was not immune to suit.
The decision in April relied on a different test for sovereign immunity that came from a 2014 ruling from the Ninth District Court of Appeals. Dr. Aila Hoss, an expert in tribal health law, said that by adopting this broader “five-factor” test, the court looked not just at the financial relationship between the organization and the tribe, but also at purpose, method of creation, control, and tribal intent.
In April, the court cited an evolved legal landscape as part of their rationale for reversing the precedent set in 2004. By deferring instead to the 2014 ruling, the Supreme Court of Alaska established tribal health consortia as “arms of the tribes.”
What This Means for Alaska, and the Rest of the Country
Under the court’s latest ruling, when THOs provide healthcare for 170,000 Alaskans, they do so as sovereign tribes, a position that distinguishes them from any other healthcare provider.
Critics of the ruling argue that it will leave employees of THOs liable to mistreatment by their employers or harassment in their workplace. The lone dissenting justice on the state supreme court wrote that “the state’s ability to protect the public will be severely limited, and thousands of Alaska workers will lose their rights.”
The State of Alaska’s brief (the federal government filed in support of the tribes), argued that granting immunity would infringe on state sovereignty and its ability to ensure worker’s rights. THOs are some of the state’s largest companies, two are among the state’s top-ten employers.
The state also worried about tax collection. Alaska does not have a reservation system which means, unlike other states, tribal organizations are subject to state taxation. The state argued that it won’t be able to enforce tax law “against entities cloaked with sovereign immunity.”
Monkman said that worries about malfeasance and lack of oversight are overstated, as federal labor laws still apply to tribal organizations. “Like any other employer, if you want to get people to work for you, you have to have a fair and equitable workplace,” he said.
As rural communities across the country struggle with high costs and low access to culturally competent care, there is abundant interest in alternative healthcare systems.
Dr. Hoss said that many rural healthcare providers have already implemented telehealth and community health aide infrastructure. Hoss also stressed the importance of the state’s inter-tribal collaboration. “Alaska has the only multi-party compact in the I/T/U[Indian Health Service/Tribal Health Services/Urban Indian Health Programs] system,” she said. The statewide wheel-and-spoke model depends on medical, legal, and administrative synchronization across thousands of miles, hundreds of tribes, and different regions to ensure continuity of care.
When asked if there is anything other rural communities can learn from adoption of the five-factor test and the primacy of tribal health in Alaska, Monkman encouraged other states to “not to be afraid of it.”
“Nationally, there is still some reluctance among non-Native people about going to an Indian hospital… but rural Alaskans currently have the best healthcare they have ever had.”