In Some Alaska Villages Up To 30% Had Hepatitis B, Which Causes Liver Cancer
Hepatitis vaccines credited as life-saving for Alaska children may be upended Hepatitis B, once rampant in Indigenous villages, has been b...
Hepatitis vaccines credited as life-saving for Alaska children may be upended
Hepatitis B, once rampant in Indigenous villages, has been brought under control in the state, but a CDC advisory committee voted to drop the vaccine recommendation for newborns

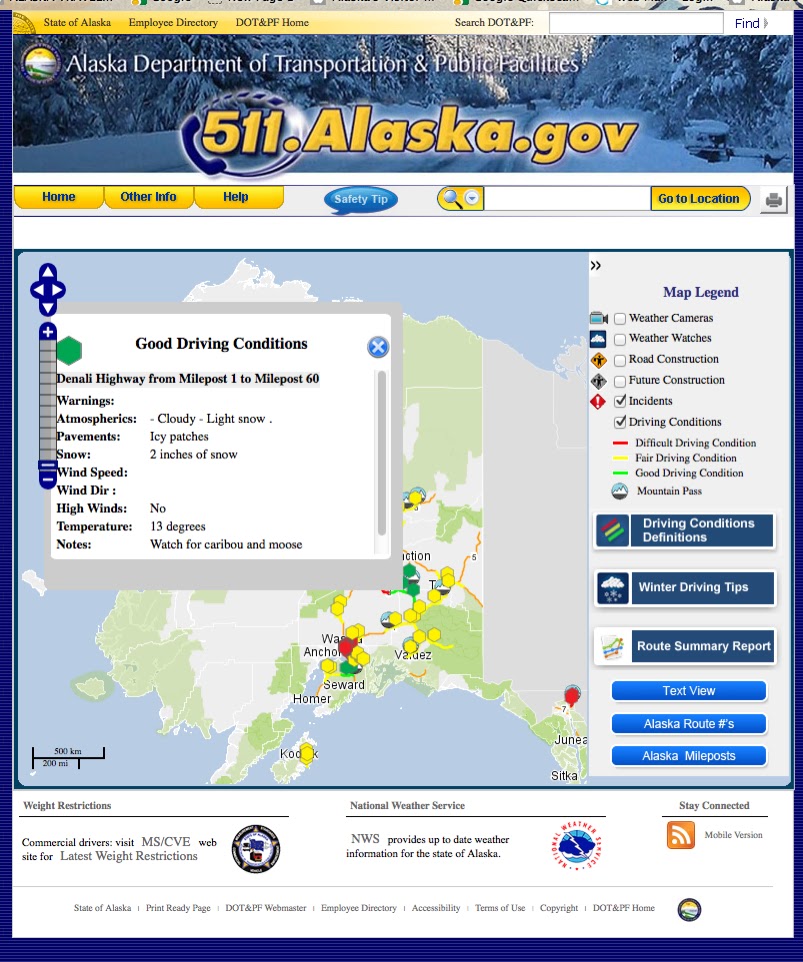
Dr. Brian McMahon, medical and research director of the liver and hepatitis program at the Alaska Native Tribal Health Consortium. stands outside at the constortium's campus on Oct. 8, 2025. McMahon tried to convince members of the federal Advisory Committee on Immunization Practices to keep in place a recommendation for universal Hepatitis B vaccination of newborns. McMahon has spoken of his experiences treating patients in Western Alaska, which in the 1970s had the world's highest rate of hepitiatis-caused childhood liver cancer. Newborn vaccinations have been critical to stopping the spread of Hepatitis B among Alaska Native children, McMahon said. (Photo by Yereth Rosen/Alaska Beacon)
Western Alaska, where almost all the residents are Indigenous, used to have the world’s highest rate of childhood liver cancer caused by Hepatitis B. After decades of screenings and vaccinations, that problem has been eliminated; since 1995, only one person under the age of 30 has been diagnosed with hepatitis-caused cancer.
Now the Trump administration is seeking to end one of the key tools credited with accomplishing that goal: Hepatitis B vaccinations of newborns.
The federal Advisory Committee on Immunization Practices on Friday voted to drop a longstanding recommendation for universal hepatitis vaccines for newborns. That is in accordance with the controversial views of U.S. Health Secretary Robert F Kennedy Jr., a vaccine skeptic who fired all members of the previous committee and appointed like-minded members to replace them.
Current federal childhood Hepatitis B vaccination guidelinesrecommend one dose of the vaccine at birth, followed by additional doses at intervals through 18 months. The recommendation for newborn vaccinations has been in place since 1991.
The advisory committee, part of the U.S. Centers for Disease Control and Prevention, determined that children under 2 months should not be vaccinated unless their mothers are infected or could be infected by Hepatitis B.
Some vaccine critics in the administration, including Kennedy and President Donald Trump themselves, argue — contradicting medical experts and years of medical research — that Hepatitis B vaccines for young children are unnecessary, claiming that it is spread primarily or exclusively through adult behavior like sex and sharing of needles for illegal drug use.
“Hepatitis B is sexually transmitted. There’s no reason to give a baby that’s almost just born Hepatitis B. So I would say wait till the baby is 12 years old and formed and take Hepatitis B,” Trump said at a Sept. 22 news conference.
Those claims are false, said Dr. Brian McMahon, medical and research director of the liver and hepatitis program at the Alaska Native Tribal Health Consortium.
There is no credible evidence of a link between the vaccine and autism of any other health problem, McMahon said.
And sexual transmissions accounted for only a tiny percentage of Alaska’s Hepatitis B cases, he said.
Aside from mother-to-infant transmissions, which occur during childbirth, Hepatitis B was predominantly spread in Western Alaska through normal daily activities. That is because, unlike the HIV virus or other hepatitis viruses, the Hepatitis B virus can live for seven days on surfaces in schools and homes, like tables and personal-grooming items.
“The virus can be found all over, on school luncheon tabletops, counters and homes,” McMahon said. “Kids have open cuts and scratches from bug bites or anything else, and then they shed millions of particles of the virus on environmental surfaces. And then another kid comes along with an open cut or scratch.”
Such risks are exacerbated in rural Alaska, he said, where homes can be crowded and people pursue traditional subsistence lifestyles with a lot of outdoor activities.
“They’re hunting, fishing, cutting up meat, etcetera, and mosquito bites are real prominent,” he said.

Alaska’s disease and vaccination success
Before the past decades of vaccination and screening, Hepatitis B was so prevalent in Western Alaska that it was classified as endemic there. It was the only part of the United States with such a classification. In some villages, 20% to 30% of the residents were infected, McMahon said.
Geography and ancient migration patterns accounted for historically high rates of the disease in Western Alaska, as well as other Indigenous regions of the Arctic.
Various strains have been carried from Asia to Alaska over millennia, according to scientists. And the remoteness of Indigenous communities meant isolation from medical services, making early diagnosis difficult in the past, allowing infections to linger and be passed down through generations, according to scientists.
In Alaska, children infected with the virus early in life had a high likelihood of winding up with chronic infections that caused serious complications later, such as liver failure. The worst cases resulted in cancer, and even death.
For McMahon, now in his 80s, treating cancer-stricken children in the Yukon-Kuskokwim region, where he worked in the 1970s, was harrowing.
One of his patients was a 17-year-old high school valedictorian. A few months earlier, she started having abdominal pains, but she ignored them.
“She was really busy with school, and she’d gotten a full ride scholarship and was excited about going to the University of Alaska, representing her community,” McMahon said.
The pains turned out to be cancer, caused by a hepatitis B infection that she had not known she had. Too sick to be flown home, she died in the Bethel hospital.
“It was horrible,” McMahon said.
Another patient was an 11-year-old boy, also diagnosed after he complained of similar abdominal pain. McMahon visited him at home, where the boy was “in horrible pain” and yellow from jaundice.
“He was just crying. He said I know I’m going to die. Just help me with my pain,’” McMahon said.
“My wife was with me. She was a public health nurse. She was in tears. The community health aid practitioner was in tears. I was fighting my tears and pulling everything I could out of my bag to try to help this patient sedate. It was just something I’ll never forget. Never.” McMahon said.
He has relayed these and other experiences to the vaccine advisory committee in hopes of persuading members to keep the infant recommendations in place.
“I said, ‘Do you want to be responsible for children getting liver cancer because of this decision?’” McMahon said. “So I’m probably not very popular right now.”
Alaska was one of the first places in the world where the Hepatitis B vaccine was used as soon as it became available in 1981.

Health officials have followed the outcomes since then, and the new study lists several achievements 40 years after universal newborn vaccination started.
Since 1995, according to the study, there have been no new symptomatic cases of Hepatitis B among Alaska Natives under 20 anywhere in the state. Since 2000, no new cases of hepatitis-related liver cancer have been identified among Alaska Natives of any age in the Yukon-Kuskokwim Delta, a region where prevalence was concentrated in the past, the study said. And follow-up surveillance has revealed that childhood Hepatitis B vaccinations remain effective for at least 35 years, the study said.
Successes are also reflected in the trend of acute hepatitis, the form of infection that is short-lived and can be cleared from the body.
There have been no identified cases of acute hepatitis among Alaska Native children since 1992, according to Johns Hopkins University. The rate of acute hepatitis among Alaskans of all ages and ethnicities dropped from 12.1 cases per 100,000 people to 0.9 per 100,000 in the 2002-2015 period, according to the state Department of Health’s epidemiology section.
Alaska’s rate of chronic hepatitis B – the long-term and persistent infection that can lead to serious liver problems – remains higher than the national average. As of 2020, Alaska’s rate of chronic Hepatitis B was 14.2 cases per 100,000 people, nearly triple the national rate of 5 cases per 100,000 people, according to a report by the state Department of Health’s epidemiology section.
McMahon said that is partly because of the legacy of infections in the older Native population, people whose childhood predated widespread vaccination, and prevalence among foreign-born residents who come from countries without widespread vaccination.
Debate over Hepatitis B risks
This year, vaccine skeptics who are members of the Advisory Committee on Immunization Practices, however, along with people who are advising the committee, have argued that the risks of Hepatitis B among children are too low to justify universal infant vaccination.
One of the officials making that argument at Thursday’s committee meeting was Dr. Cynthia Nevison, a vaccine skeptic hired as a CDC consultant. She contradicted McMahon’s description of children spreading the virus through casual contact with contaminated surfaces – a process known as “horizontal transmission.”
“There’s very little evidence that horizontal transmission has ever been a significant threat to the average American child, and the risk probably has been overstated,” she said at the meeting. Also overstated, she said, are the risks of “vertical transmission,” the viral transmission between mothers and their newborns.
The committee’s new recommendation must be approved by the CDC administrator before it becomes federal policy.
McMahon said that no matter how national policy might change, Alaska Native tribal health organizations will continue administering Hepatitis B vaccines to newborns.
“I know they’re not going to stop. Even if they have to pay for it. They’re so aware of this,” he said.
His fears, he said, are for low-income families who depend on free vaccinations through state programs that might lose funding and for parents who are getting conflicting messages that may lead to conclusions that the vaccine is not necessary.
“It could be a real mess,” he said.