Edna Charley, Former Executive Director Of CRNA, Health Aide, Mother & Grandmother
IN MEMORY... In Her Own Words: Edna Charley Spoke Of What Is Possible As A Community Health Aide In An Alaskan Village Edna Charley, a long...
IN MEMORY...
In Her Own Words:
Edna Charley Spoke Of What Is Possible As A Community Health Aide In An Alaskan Village
Edna Charley, a longtime resident of the Copper Valley with close family ties to many people who live here, has died. Any further family memorials meant for the public will be printed later.
Always dedicated to serving her community and nurturing her large family, Edna had a firm grasp on what was important. Her lifelong interest in swim programs, dental care, river safety, children and diabetes all stemmed from earlier programs at CRNA which she oversaw as head of the organization in the 80s.
The following narrative is from a State of Alaska document over 20 years ago, entitled "Community Health Aides; Alaska's Unique Health Care Providers." In the document, Edna Charley was chosen from all the health aides in Alaska to describe what it means to be a Community Health Aide Practitioner. This was written shortly before her retirement in May 2002.
Edna Charley: "We Have To Be Role Models...As Well As Teachers"
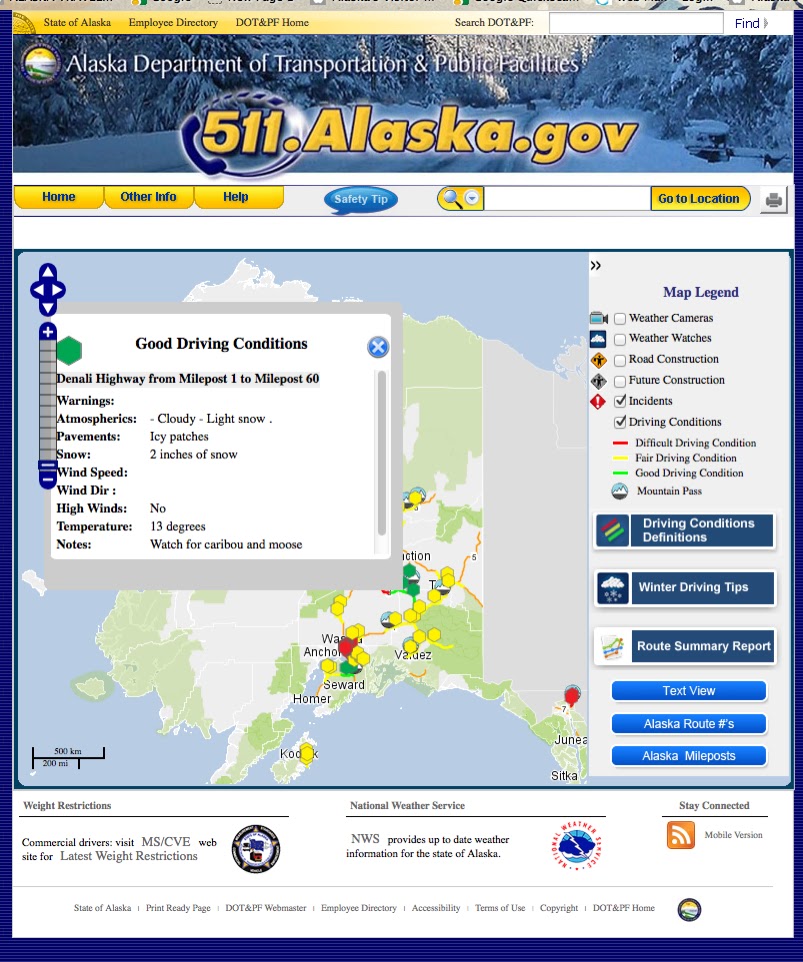
“It was 1976 and the health aide program was just getting started in Glennallen. They needed somebody and they knew I had been a nurse. My kids wanted to move up there. They grew up in Anchorage, but they liked village life. So I agreed to do it.
“There was no clinic. I worked out of my house and out of my car. All we had was a little cabin. I just moved into that little cabin and all my medicines were in that little black bag. I kept it in my trunk. That was the only safe place to lock it up.
“Chistochina is a tiny village—33 people. I’d call the kids in for fluoride treatment, do home visits and take blood pressures. I was on the village council, too, so I kind of pushed for a clinic. We took one of the older houses there and got some money to fix the inside. There was no running water and no sewer. The heat was propane. No refrigerator, but it was cool enough in there we didn’t need one. I liked it, but because it was on the highway system, a lot of people went to the doctor. It wasn’t that much of a challenge. But I got promoted and became a health aide supervisor.
“I moved back here to Kake, my hometown, October 6, 1987. It was a major change. Having 700-800 people here, more in the summer. When I first came I was the only health aide. But we had real good docs. They were supportive of the health aides. I appreciated that because I’ve worked where they weren’t supportive, where they question your abilities and your knowledge. It means a lot to me that I’ve had that support.
“Moving to the village to be a health aide, I had to learn the political part just to get a clinic. I was involved in the village council. I was on the health board, service unit board, and Native health board. And then, AFN (Alaska Federation of Natives), too. I learned all about communication. I enjoyed that. I was on the city council for a while, too. Always with the same direction: health and safety.
“I like the direct patient care. I resisted stuff like the computer. I didn’t like the idea of patient information being on there. But it really helped.
“The equipment—the digital camera and video otoscope—helps a lot. Being able to get directions right away from the doctors. They get it and call us right back. Helps a lot and saves traveling money. And the polycam. It’s like a TV where you can have a meeting and camera and everyone can talk. It’s not delayed and it’s not jerky. It’s live; it’s really nice. We use that for getting directions on patient care.
“The major changes are the technology. I was thinking about that little black bag, the old-fashioned doctor’s bag. We have a lot more drugs. You could never carry them in the old black bag! We have a lot more vaccines, and the schedule is always changing. We have x-ray. There’s a lot to learn. Our manual used to be a little yellow book. Now it’s three books. Another difference is getting more dental care here. That’s what we do, too—we point out what we think we need, like the increase in dental care.
“I think what really helped me was having the doctors being supportive and having confidence in my ability. Makes a big difference. And then the staff here, we get along and we’re supportive of each other. And we laugh a lot. Many things to laugh about! I think my own personal faith is what kept me going. And, it just happens that the staff here, too, has strong faith and we draw on each other a whole lot. My grandchildren help a lot, too. They help you realize life goes on.
“The part I like, besides the direct patient care, is the education and prevention. The ‘Kids Don’t Float Program,’ the ‘Peacemaking Circle.’ We used to go to the school to give health education, sex education, that kind of thing. I think it is a major part of our job.
We try to influence the health, the well-being of the community. We started community clean up. It still goes on. We did a diabetes screening—went door to door. They wouldn’t come to the clinic. When I came we had three diabetics. Now there are 28. That’s a shift, too. But I think we are making people become more aware of those kinds of things. That’s our responsibility, not just taking care of the cold or the laceration.
We pushed for the swim program, too. That’s going on this summer. It only makes sense. We live right here, by the water. If people are fishing for salmon, they are on the water. We’re lucky that nothing’s happened, but we don’t want to wait for something to happen.
“We have to be role models, too, as well as teachers. It doesn’t make your work very strong if you aren’t living it yourself. You can’t just preach about things, especially in small communities. You can’t teach about alcohol abuse if you’re abusing it yourself. We are involved with the Healing Heart Circle, something positive in town.
“I think the health aides, the ones who hang in there, are the same kind of people who are involved in the community. You have to know all that, what’s going on in the community. We have to know our community pretty well.
“Having the self-determination for the tribe, and being responsible for our own healthcare, have made a big difference. When I grew up here, there was nothing. I remember suffering with ear infections, toothaches. Most of the babies were born here. Big difference. Not that long a time, really. One lifetime.”