Emergency Medical Services In Rural America, Where People Are Older, Sicker, Poorer... And More Isolated
EMS Services in Rural America: Challenges and Opportunities Nikki King, MHSA, Marcus Pigman, MHA, Sarah Huling, BS- ARRT, ARDMS, and Bria...
EMS Services in Rural America: Challenges and Opportunities Nikki King, MHSA, Marcus Pigman, MHA, Sarah Huling, BS- ARRT, ARDMS, and Brian Hanson, PhD
Executive Summary:
Across the United States, about 57 million people, or 18% of the total population, call rural communities home1. While rural America may conjure idyllic images of family farms, the truth is far more staggering. Rural Americans, on average, tend to be older, sicker, and poorer2. The Centers for Disease Control (CDC) concludes in a recent report that “percentages of potentially excess deaths among persons aged <80 years from the five leading causes were higher in nonmetropolitan areas than in metropolitan areas”3. 26.7% of rural children live in poverty, a nearly 7% increase in recent years due, for the most part, to declining average family incomes4. In addition to declining incomes, the gap in life expectancies between rural and urban Americans has also been widening. A study of data that ranged from 1969-2009 found that the average life expectancy of rural Americans was just 76.7, nearly 2.5 years below that of their urban counterparts5. However, in some rural regions, the difference between urban and rural life expectancies is as much as 20 years6. Despite this clear need for increased healthcare access in rural areas, only 9% of practitioners in the U.S. work in rural America7. Additionally, rural hospitals are facing closure crisis, with about 41 percent of Critical Access Hospitals (CAHs) facing negative operating margins, which further decreases possible points of care for people with a pronounced need 8 9.
In the face of this glaring healthcare disparity, rural Emergency Medical Services (EMS) often become the only guaranteed access to health services, and ultimately, the safety net for underserved rural communities. However, dwindling population, losses in the volunteer workforce, and decreased reimbursement threaten continued access to these services. Nearly one-third of rural Emergency Medical Services (EMS) are in immediate operational jeopardy10. Therefore, action must be taken to secure access to, and the quality of, this vital service for rural Americans.
Myriad Challenges for Rural EMS Providers:
Inequality in access to healthcare between rural and urban Americans is apparent across a range of factors, as evidenced by higher rates of potentially excess deaths among rural Americans from the five leading causes of death than their urban counterparts (see Figure 1 below)11. This disparity is particularly evident in the opioid overdose epidemic. One of the major contributing forces to the stark decrease in life expectancies for rural Americans is that they are more than 50% more likely to die of trauma-related causes12. One of the most endemic trauma- related causes of death is drug overdose.
The CDC finds that from 1999 to 2015, the opioid death rates in rural areas of the U.S. have quadrupled among those 18-25 years old and tripled for females”13. In fact, the overall rate of drug overdose in rural areas has surpassed that of metropolitan areas over roughly the last two decades. Other research finds that “drug overdose death rates (per 100,000 population) for metropolitan areas were higher than in nonmetropolitan areas in 1999 (6.4 versus 4.0), however, the rates converged in 2004, and by 2015, the nonmetropolitan rate (17.0) was slightly higher than the metropolitan rate (16.2)”14. Another study finds that while the odds of being administered naloxone (a treatment to counteract drug overdose, also known by its brand name Narcan) by an EMT in rural areas was higher than urban areas, the drug overdose death rate still remains higher overall15.
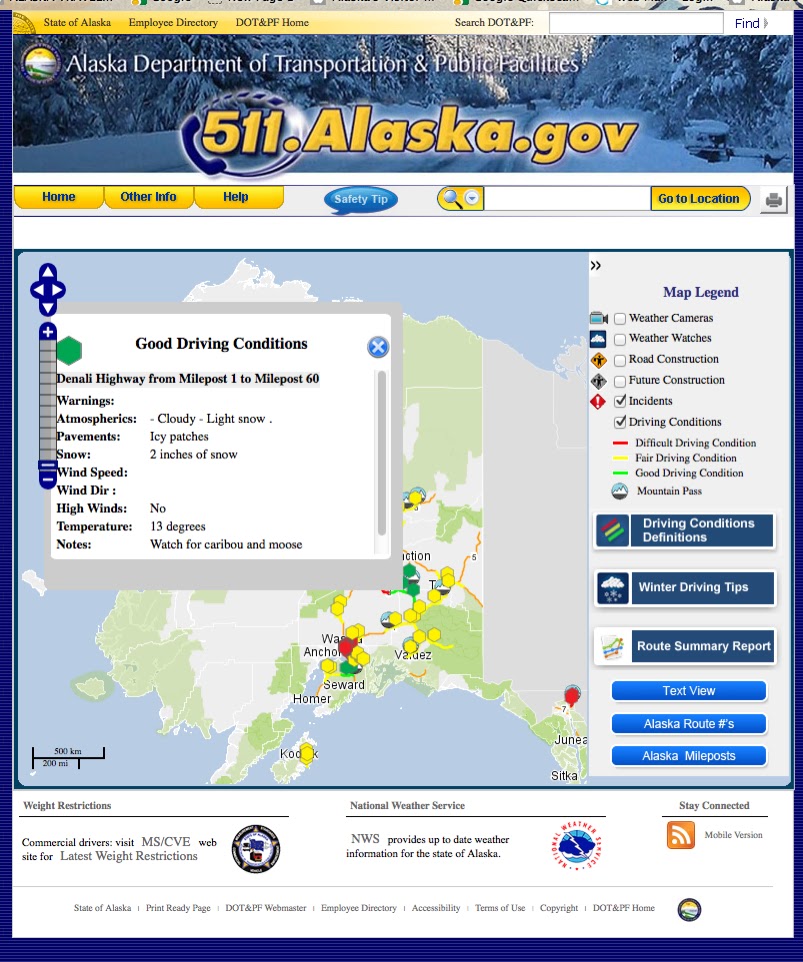
It is very common for EMS units in rural parts of the U.S. to have sparsely populated coverage areas that stretch over large distances and challenging terrain. Time and distance traveled for EMS personnel to respond to a call will typically be much greater in rural areas than urbanized areas17. This is especially true for EMS providers that are located in counties where an existing hospital is not available. The large coverage areas, travel distances, and increased demand for time spent with the patient can lead to significant impacts on patient outcomes and survival rates. For example, the fatality rate from a vehicular accident in a rural area is almost twice as high when compared to an urban area18. Faster EMS response times create better patient outcomes19. Many EMS providers set a goal of having a response time of 8 minutes or less for advanced life support (ALS) units when dealing with life-threatening events20. However, this may become an unattainable goal for many rural EMS providers as travel time and distance to the patient location alone can far exceed an 8-minute threshold.
One of the largest contributing factors to the disparity in mortality rate from traumas, such as overdose, for rural residents (discussed above) is travel time and distance to trauma centers. In fact, research finds rural residents are significantly more likely than non-rural residents to die following traumatic injury, and that disparity varies by trauma center designation, injury severity, and US Census region21. The authors of this study also found regional differences in pre-hospital care and trauma system organization leads to disparity in mortality between rural and non-rural residents from trauma being the greatest in the South and Midwest. Using national data from National Emergency Medical Services Information System (NEMSIS), we find that on average, EMS total call time (from time unit is dispatched, the patient arrives at the hospital, and the EMS unit is ready for the next call) in rural areas of the U.S. are nearly 20 or 30 percent higher than suburban and urban areas, respectively (see Figure 2 below) 22. Another study of Alabama finds in the case of fatal automobile accidents was over 40% higher in rural areas than urban23. In 2007, 24% more of the population had to travel farther to the nearest trauma center. In fact, travel time to any medical facility was 36% longer for rural residents than for other Americans24.
In the case of opioid overdoses, the patient typically experiences depressed respiratory function. The 9.4 extra minutes, on average, that it takes to transport the patient to the local hospital is often the difference between life and death25. In many states, over the counter nasal Naloxone has been made available to community bystanders, however EMS providers are still the primary source of Naloxone administration prior to hospital arrival26. Naloxone administration is standard protocol for paramedic and advanced EMS personnel27. However, most states do not allow basic life support providers to administer naloxone28. With the opioid addiction, and related overdoses, in the U.S. reaching epidemic scale, pressures on the EMS system will continue to grow.
Exacerbating the problem of longer times and distances for EMS transport is the ongoing critical access hospital (CAH) closure crisis. 82 rural hospitals have closed in the U.S. since 201029. CAHs are small, rural hospitals that have 25 or fewer inpatient beds, have average stays of less than 96 hours, provide 24/7 emergency car, and are 35 miles from the next nearest hospital, unless otherwise designated as a CAH by their respective state. When rural hospitals close, the transport times from scene to hospital greatly increase in more remote parts of the U.S., where the distance between hospitals can already be over 90 miles. Research on the recent increase in hospital closures finds market factors and financial difficulties such from declining population served, negative profit margins, and reduced Medicare reimbursement rates due to Congressional budget sequestration, high levels of debt, and low levels of capital to be significant contributing factors to closure30.
Workforce Woes:
Rural EMS services are more dependent on volunteers than their urban counterparts. A national survey of local EMS directors in rural and urban areas finds rural agencies were more likely to be staffed by volunteers only (53% for isolated small rural vs. 14% for urban, see Figure 3)31. In some rural parts of the country (tending to be those more sparsely populated) it is estimated that volunteers cover more than 90 percent of EMS calls32. More than two-thirds (69%) of rural EMS directors surveyed in 2015, reported that they have a problem recruiting and/or retaining volunteers, with more than half (55%) reported that recruitment and retention problems are the same or are getting worse33. When asked open-ended questions about staffing challenges, rural EMS directors cited:
● “The rural population base is small. There are few employers in many areas and many people work out-of-town, making it impossible for them to volunteer during the day.
● It is difficult to provide weekend coverage. There are too many competing demands for volunteers with families.”
Funding and reimbursement difficulties from third-party payers, along with low call volume, creates a situation in which many EMS providers in rural areas must rely upon all- volunteer workforce to financially maintain operations34. Recruitment and retention of trained personnel to serve on a volunteer basis can be a very difficult and inefficient process for EMS services in rural communities. Serving on a volunteer basis results in a situation in which the person must maintain other means of employment to meet their personal financial needs35.
Attracting new EMS staff and retaining current staff is critical to ensuring quality of care for those who live in rural areas. One of the most efficient ways to attract new staff is to increase the supply of EMS staff from which to recruit through expanded training opportunities. Despite prior commitments to their paid employment and family obligations, EMS personnel are still required to routinely attend various education and training sessions to maintain their skills and certifications36. Time and resource availability to meet these training needs can become overwhelming to the volunteer staff. Therefore, research and sustainable funding are needed to increase both the number of full-time paid opportunities and paid training for volunteers to alleviate recruiting and retention difficulties for rural EMS units.
Many of these workers spend hundreds of dollars out of pocket for certification and live with no healthcare coverage because they know that, without them, their communities would not have adequate EMS coverage. In situations where adequate coverage cannot be achieved, long wait times significantly reduce outcomes for rural patients. In order to combat the rapidly shrinking volunteer force, some forces have moved to paying their volunteers. Typically, these forces either pay by the number of runs the staff member goes on, or for stand-by time37. Among EMS forces who do not pay their volunteers, about 1/3 are considering moving to paid volunteers in the near future with the primary reason the forces listed for not moving to paid personnel is a lack of funds38.
A 2011 publication titled The EMS Workforce Agenda produced by the U.S. Department of Transportation National Highway Traffic Safety Administration, lists four key components that were critical to EMS workforce development: health, safety and wellness of the EMS workforce; education and certification; data and research; workforce planning and development39. Standardized data is an essential element in the development of these four elements, which should be collected regularly at both the local and state levels and reported nationally40. Lack of standardized and uniform EMS data at both the national and state levels creates a barrier for developing operational improvement strategies, along with increased provider safety and patient care41. Data and research plays an important role in the development of an effective EMS workforce, which is the principal component of any EMS system42.
Leadership training opportunities and requirements for EMS Service Managers should also be reviewed. A study in 2014 by the National Association of State Emergency Medical Services Officials found that almost half of the states in the U.S. do not offer education programs for leadership education. In the states that do provide training opportunities for leadership, only 15 percent make the training mandatory43. Educational and training opportunities for EMS Service Medical Directors are another area that should be reevaluated. In most states, only a physician can serve as the Medical Director of an EMS service; however, a few states do allow for either a Physician Assistant (PA) or Advanced Practice Registered Nurse (APRN) to serve in that capacity. Medical Directors are generally responsible for guidance, medical oversight and quality assurance for the practice of local paramedic and EMTs affiliated with an ambulance service44. As with leadership trainings for EMS Service Managers, almost 50% of states in the U.S. do not offer any educational or training programs for Medical Directors either. With the states that do provide training opportunities for Medical Directors, only 52% make the training mandatory45. About half of rural EMS medical directors are volunteers, only about 40 percent of directors directly observe or participate in unit activities (through training, testing, or accompanying a unit on a call) on a least a monthly basis46.
Challenges of Inconsistent Funding:
The cost per transport is higher in rural areas because the base costs of “maintaining readiness” are sunk costs, yet with lower volumes there is less of a funding stream to offset costs47. Both low-volume and high-volume ambulance transports require up-to-date and maintained ambulance and crew. However, the increased volume in urban and suburban areas increases likelihood of recuperating of operational costs. As a downstream effect of lower volumes, rural ambulances have higher costs per transport and more associated bad debt.
Although rural areas typically experience fewer emergency events, adequate funding for equipment, staffing and training can be a major factor in the delivery of this much needed service. Reimbursement for EMS services are typically linked to call volume therefore it is common for rural EMS providers to depend heavily on volunteer Emergency Medical Technicians (EMTs) to meet staffing needs on a limited and fixed budget. Studies have shown that over 60% of rural EMS providers rely on volunteers for EMT-Intermediates or EMT- Paramedics48. Almost 70% of rural EMS providers report having difficulty in recruiting volunteers to adequately meet staffing needs49.
The same report shows rural EMS agencies report a mixture of funding sources, with 83% reporting multiple sources funding in one survey. Around 62 percent of agencies report billing patients, insurers and/or hospitals directly. Meanwhile, three-quarters of rural EMS agencies are funded by local/county funds and around 60 percent report community fundraising efforts (think pancake feeds and fish frys). This hodgepodge of funding sources does not help to mitigate recruiting and retention difficulties, nor does it provide a consistent revenue stream that can help maintain up-to-date equipment and or software. And due to EMS services of often being funded through myriad local sources, state and federal legislators may reluctant to take on new spending obligations to shore up fading local units. One state EMS director we spoke to described it thusly, “State and federal officials must think ‘Why pay for what you have always gotten for free?’”
7
In addition to relying on already limited community funds as a primary mechanism of support, rural EMS services are plagued by difficulties in billing practices. Inadequate access to care leads to many “cold calls”, or calls where no hospital treatment was required, leading to no transport services to bill. Additionally, when Naloxone is used to revive a patient, many patients will refuse transportation to the hospital for fear of legal ramifications. This leads the EMS service to lose the sunk costs associated with the run as well as the cost of the Naloxone because they can only bill for a successful transport to a medical facility.
Decreasing populations (particularly in working age adults) across rural America leads to and the previously discussed declining availability of volunteers, but also a decreasing community fundraising pool50. Rural areas are also more likely to have decreased local access to EMS training for what is primarily a volunteer position. Recruits have to travel farther to receive training they may not be reimbursed for a part-time job they unlikely to be paid for. Additionally, sparser populations do not decrease the fixed costs of the ambulance services, and increases the variable costs per run. These factors combined with the significant chronic care issues, such as increased trauma incidence from high-risk employment and automobile collisions, and the rise of the opioid epidemic have created an untenable financial landscape51. Over 1/3 of rural EMS services reported being pessimistic about their ability to continue to offer services in the future52. An additional 20% reported that they were only 50% sure of their continued financial viability53.
Fragmented Coordination of Service:
According the 2011 National EMS Assessment there are an estimated 21,283 credentialed EMS agencies in the U.S, with a majority managed at the sub-county level. “Home Rule” refers to the process of state-level governments delegating power to smaller units of government such as towns, townships, villages, etc55. Home Rule, as it relates to EMS services, creates autonomous emergency squads in specific areas. In communities without Home Rule, larger more coordinated systems of EMS services have emerged. This cohesiveness allows for more consistent quality of care. Consolidation also allows for better distribution of certain sunk costs, such as administrative costs as well as more efficient use of resources such as dispatch systems, better disaster preparedness, improved quality oversight, consistent medical protocols, and more integrated systems of care with healthcare providers in the community56.
The inherent variability in quality of care and the challenges to EMS services’ continued viability were acknowledged in the EMS Agenda for the Future as far back as 1996. Since then, there have been many advancements in education and training standards for emergency service providers, as well as advancements in scope of practice. Despite these improvements, however, many rural areas still suffer from fragmented and disorganized EMS coverage. For example, in Batesville, Indiana, with a population of around 6,000, an emergency call could be answered by any one of 6 service providers. These providers practice autonomously, and therefore do not share volunteers, best practices, or quality reporting data. Additionally, with many EMS services relying on community buy-in to fund their operations, all 6 of these services tapping the same small community’s resources to remain functional. Despite the overlap in services, due to each squad’s inherently small size, losing even one would create a large gap in coverage for the people living in that community.
Conclusion
Rural Americans are older and sicker than their urban counterparts, creating unique challenges for EMS providers57. Additionally, due to Home Rule and a limited funding pools, these providers have reduced operational efficiencies and fewer resources with which to provide these lifesaving services58. In rural areas, where travel times to the nearest medical provider are already higher, a fully optimized EMS force is crucial to ensuring good patient outcomes59.
Recommendations
The following are recommendations to improve the quality and consistency of care as well as improve the long-term financial viability of EMS services:
● Research funding is needed to examine how to efficiently and sufficiently reimburse low volume and rural EMS services to improve quality of care and guarantee long-term viability for local EMS agencies. There needs to be reliable funding in order to continue these essential services.
9
● Further research is needed on systems of storage and distribution for nasal naloxone in low volume communities to combat opioid overdoses.
● Implementation of a large-scale EMS data reporting and monitoring system is need to formulate more efficient and effective service provision in rural areas. Funding is needed both to acquire the needed resources (equipment, software, and maintenance) and to and hire administrative support personnel to implement this system, as well as to aid EMS providers in securing reimbursement for the services they provide.
● Research grant programs are needed to fund the study of best practices and innovations from local EMS agencies across the U.S. In turn, grants can be offered to states authorities, as well as, local EMS officials that adopt innovations and best practices found through this research to encourage broader application of best practices.
● Further study needed on how EMT services affect rural hospitals’ financial bottom line and how such hospitals are reimbursed for EMS services.
10
References:
1
October 12, 2017 2 National Rural Health Association. What’s different about rural health care?
http://www.ruralhealthweb.org/go/left/about-rural-health. Published 2010. Accessed September 9, 2017.
3 Moy, Earnest; et al. Centers for Disease Control and Prevention. Leading causes of death in nonmetropolitan and metropolitan areas —United States, 1999–2014. https://www.cdc.gov/mmwr/volumes/66/ss/ss6601a1.htm?s_cid=ss6601a1_w Published January 13, 2017. Access September 9, 2017.
4 Hertz, T. and Farrigan, T. Understanding the rise in rural child poverty, 2003-2014. Economic Research Report. 2016;208, pp.1-3.
5 Singh, G. and Siahpush, M. Widening rural–urban disparities in life expectancy, U.S., 1969–2009. American Journal of Preventive Medicine. 2014;46(2), pp.e19-e29
6 Dwyer-Lindgren, L., Bertozzi-Villa, A., Stubbs, R., Morozoff, C., Mackenbach, J., van Lenthe, F., Mokdad, A. and Murray, C. Inequalities in Life Expectancy Among US Counties, 1980 to 2014. JAMA Internal Medicine. 2017;177(7), p.1003
7 Rosenblatt, R. Physicians and rural America. Western Journal of Medicine. 2000;173(5), pp.348-351
8 Kaufman, B, Thomas, S, Randolph, R, Perry, J, Thompson, K, Holmes, G, Pink, G. The rising rate of rural hospital
closures. The Journal of Rural Health. 2016; 32(1): 35-43
9 Topchik, Michael. The Chartis Group - Chartis Center for Rural Health. Rural relevance 2017: assessing the state of rural healthcare in America. http://www.ivantageindex.com/2017-rural-relevance-study/ Published 2017. Accessed December 20, 2017.
10 Freeman, V., Rutledge, S. Hamon, M. , Slifkin, R. Rural volunteer EMS: reports from the field. North Carolina Rural Health Research and Policy Analysis Center. Final Report No. 99. August 2010. http://www.shepscenter.unc.edu/rural/pubs/report/FR99.pdf
11 Moy, Earnest; et al. Centers for Disease Control and Prevention. Leading causes of death in nonmetropolitan and metropolitan areas —United States, 1999–2014. https://www.cdc.gov/mmwr/volumes/66/ss/ss6601a1.htm?s_cid=ss6601a1_w Published January 13, 2017. Access September 9, 2017.
12 Ibid.
13 Noonan, R. Centers for Disease Control and Prevention. Public Health Matters Blog. Rural America in crisis: The changing opioid overdose epidemic. https://blogs.cdc.gov/publichealthmatters/2017/11/opioids/ Published November 28, 2017. Accessed December 20, 2017.
14 Mack KA, Jones CM, Ballesteros MF. Illicit Drug Use, Illicit Drug Use Disorders, and Drug Overdose Deaths in Metropolitan and Nonmetropolitan Areas — United States. MMWR Surveill Summ 2017;66(No. SS-19):1–12. DOI: http://dx.doi.org/10.15585/mmwr.ss6619a1
Health Resources and Services Administration. Defining rural population.
https://www.hrsa.gov/ruralhealth/aboutus/definition.html Published 2017.
11
15 Faul, M., Dailey, M., Sugerman, D., Sasser, S., Levy, B. and Paulozzi, L. (2015). Disparity in Naloxone Administration by Emergency Medical Service Providers and the Burden of Drug Overdose in US Rural Communities. American Journal of Public Health, 105(S3), pp.e26-e32.
16 Moy, Earnest; et al. Centers for Disease Control and Prevention. Leading causes of death in nonmetropolitan and metropolitan areas —United States, 1999–2014. https://www.cdc.gov/mmwr/volumes/66/ss/ss6601a1.htm?s_cid=ss6601a1_w Published January 13, 2017. Access September 9, 2017.
17 Jarman, M, Castillo, R, Carlini, A, Kodadek, L, Haider, A. Rural risk: geographic disparities in trauma mortality. Surgery. 2016; 160 (6) 1551-1559.
18 Gonzalez et al. (2009). Does Increased Emergency Medical Services Prehospital Time Affect Patient Mortality in Rural Motor Vehicle Crashes? A Statewide Analysis. The Journal of Emergency Medicine, 37(1), pp.109-110
19 Ibid
20 Moy, Earnest; et al. Centers for Disease Control and Prevention. Leading causes of death in nonmetropolitan and metropolitan areas —United States, 1999–2014. https://www.cdc.gov/mmwr/volumes/66/ss/ss6601a1.htm?s_cid=ss6601a1_w Published January 13, 2017. Access September 9, 2017.
21 Jarman, M, Castillo, R, Carlini, A, Kodadek, L, Haider, A. Rural risk: geographic disparities in trauma mortality. Surgery. 2016; 160 (6) 1551-1559
22 National Emergency Medical Services Information System. 2015 Public Use National EMS Database https://nemsis.org/view-reports/public-reports/ems-data-explorer/ Published 2015. Access December 21, 2017.
23 Gonzalez et al. (2009). Does Increased Emergency Medical Services Prehospital Time Affect Patient Mortality in Rural Motor Vehicle Crashes? A Statewide Analysis. The Journal of Emergency Medicine, 37(1), pp.109-110
24 Blanchard, I., Doig, C., Hagel, B., Anton, A., Zygun, D., Kortbeek, J., Powell, D., Williamson, T., Fick, G. and Innes, G. Emergency medical services response time and mortality in an urban setting. Prehospital Emergency Care. 2012; 16(1):142-151.
25 Ibid.
26 Davis, C., Southwell, J., Niehaus, V., Walley, A. and Dailey, M. (2014). Emergency medical services naloxone
access: A national systematic legal review. Academic Emergency Medicine, 21(10), pp.1173-1177. 27 Ibid.
28 Ibid.
29 The Cecil G. Sheps Center for Health Service Research - University of North Carolina. 2016. “82 Rural Hospital Closures: January 2010 - Present” http://www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospital- closures/ Published 2017. Accessed December 20, 2017.
30 Kaufman, B, Thomas, S, Randolph, R, Perry, J, Thompson, K, Holmes, G, Pink, G. The rising rate of rural hospital closures. The Journal of Rural Health. 2016; 32(1): 35-43
12
31 Patterson DG, Skillman SM, Fordyce MA. Prehospital Emergency Medical Services Personnel in Rural Areas: Results from a Survey in Nine States. Final Report #149. Seattle, WA: WWAMI Rural Health Research Center, University of Washington, August 2015
32 Ibid.
33 Freeman, V., Rutledge, S. Hamon, M. , Slifkin, R. Rural volunteer EMS: reports from the field. North Carolina Rural Health Research and Policy Analysis Center. Final Report No. 99. August 2010. http://www.shepscenter.unc.edu/rural/pubs/report/FR99.pdf Accessed December 20, 2017.
34 Ibid.
35 Ruralhealthinfo.org. Rural Emergency Medical Services (EMS) and Trauma Introduction - Rural Health Information Hub. https://www.ruralhealthinfo.org/topics/emergency-medical-services Published 2017. Accessed 12 Oct. 2017.
36 Ibid.
37 Freeman, V., Rutledge, S. Hamon, M. , Slifkin, R. Rural volunteer EMS: reports from the field. North Carolina Rural Health Research and Policy Analysis Center. Final Report No. 99. August 2010. http://www.shepscenter.unc.edu/rural/pubs/report/FR99.pdf Accessed December 20, 2017.
38 Ibid.
39 EMS.gov. The emergency medical services workforce agenda for the future https://www.ems.gov/pdf/2011/EMS_Workforce_Agenda_052011.pdf Published 2017. Accessed 12 Oct. 2017.
40 Ibid.
41 EMS.gov. EMS Data Initiatives. https://www.ems.gov/emsdata.html. Published 2017. Accessed October 12, 2017
42 EMS.gov. The emergency medical services workforce agenda for the future https://www.ems.gov/pdf/2011/EMS_Workforce_Agenda_052011.pdf Published 2017. Accessed 12 Oct. 2017.
43 Emergency Medical Services Leadership Education. https://www.nasemso.org/Projects/RuralEMS/documents/JCREC-Leadership-Education-Compendium_v2.0-Final- Draft_2014-2015.pdf Published 2014. Accessed 12 Oct. 2017.
44 EMS.gov. The emergency medical services workforce agenda for the future https://www.ems.gov/pdf/2011/EMS_Workforce_Agenda_052011.pdf Published 2017. Accessed 12 Oct. 2017.
45 Ibid.
46 Patterson DG, Skillman SM, Fordyce MA. Prehospital Emergency Medical Services Personnel in Rural Areas: Results from a Survey in Nine States. Final Report #149. Seattle, WA: WWAMI Rural Health Research Center, University of Washington, August 2015
47 United States Government Accountability Office. Costs and medicare margins varied widely; transports of beneficiaries have increased. http://www.gao.gov/assets/650/649018.pdf Published 2012. Accessed 12 Oct. 2017.
13
48 Freeman, V., Rutledge, S. Hamon, M. , Slifkin, R. Rural volunteer EMS: reports from the field. North Carolina Rural Health Research and Policy Analysis Center. Final Report No. 99. August 2010. http://www.shepscenter.unc.edu/rural/pubs/report/FR99.pdf
49 Ibid. 50 Ibid.
51 Jarman, M, Castillo, R, Carlini, A, Kodadek, L, Haider, A. Rural risk: geographic disparities in trauma mortality. Surgery. 2016; 160 (6) 1551-1559.
52 52 Freeman, V., Rutledge, S. Hamon, M. , Slifkin, R. Rural volunteer EMS: reports from the field. North Carolina Rural Health Research and Policy Analysis Center. Final Report No. 99. August 2010. http://www.shepscenter.unc.edu/rural/pubs/report/FR99.pdf
53 Ibid.
54 Federal Interagency Committee on Emergency Medical Services. 2011 National EMS Assessment. U.S. Department of Transportation, National Highway Traffic Safety Administration, DOT HS 811 723, Washington, DC, https://www.ems.gov/pdf/811723-National-EMS-Assessment-2011.pdf Published 2012. Accessed, November 20, 2017.
55 Berwick DM, Downey AS, Cornett E. A national trauma care system: integrating military and civilian trauma systems to achieve zero preventable deaths after injury. Washington, DC: The National Academies Press; 2016
56 Ibid.
57 Singh, G. and Siahpush, M. (2014). Widening Rural–Urban Disparities in Life Expectancy, U.S., 1969–2009. American Journal of Preventive Medicine, 46(2), pp.e19-e29.
58 Berwick DM, Downey AS, Cornett E. A national trauma care system: integrating military and civilian trauma systems to achieve zero preventable deaths after injury. Washington, DC: The National Academies Press; 2016
59 Becknell, J. SOUTH DAKOTA EMERGENCY MEDICAL SERVICES SURVEY AND LISTENING SESSIONS REPORT.https://doh.sd.gov/documents/EMS/2016FinalSD-EMS-Survey-Report.pdf. Published 2016. Accessed October 12, 2017.
14